
The birth control implant, available in over 100 countries, is a highly effective form of hormonal birth control that many people find to be a convenient method of preventing pregnancy. The implant is inserted into the arm and can be kept for up to five years.1 Using a synthetic version of the hormone progestin rather than estrogen, the implant stops ovulation and thickens the walls of the uterus so that sperm cannot reach an egg. Since the implant only inhibits pregnancy, it is not capable of preventing the spread of sexually transmitted infections (STIs), so barrier methods of contraception are recommended for use in conjunction with the implant. There are both benefits and risks to using the birth control implant, and one should consult with a healthcare professional about using the implant.
What Is the Birth Control Implant?
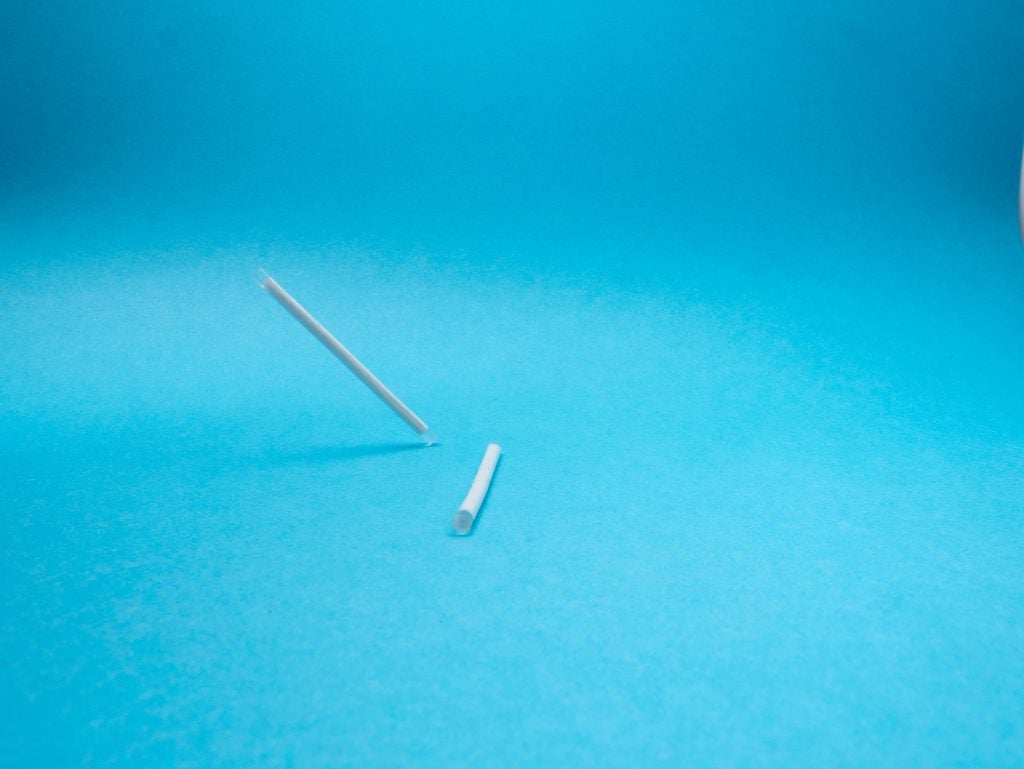
The birth control implant, which is sold currently in the United States as Nexplanon®, is a form of hormonal birth control that is inserted subdermally (under the skin) into an individual’s upper arm. Sometimes, the birth control implant may be referred to as Implanon®, which is a slightly older version of Nexplanon®.2 The device is made up of a flexible piece of plastic about the size of a matchstick and is fully reversible.3
The implant is a unique and viable method for many individuals due to its ease of use and high success rate. Nexplanon users do not have to remember to take a pill or replace their birth control frequently. The implant is over 99% effective, making it one of the most effective forms of birth control.3 Once it is inserted, no further steps are needed to prevent pregnancy.2 The insertion of the birth control implant can be performed in a few minutes during a routine visit to a healthcare provider without needing any major surgery. The implant functions with the use of progestin, making it an estrogen-free method, which is optimal for many users who may be estrogen-sensitive/reactive.4
How Is It Inserted?
Before having the birth control implant inserted, it is important to inform your doctor of any previous hormonal contraceptive use and of any abortions or miscarriages you might have had. Furthermore, your doctor might perform a physical examination and/or give you a pregnancy test. This information will help your doctor time the insertion of the implant to your menstrual cycle. Depending on when implanted during a person’s menstrual cycle, it may be necessary to use a barrier method of contraception for the week following insertion.4 More specifically, if the implant is inserted five days into the menstrual cycle, it will be effective immediately. If it is inserted at any other time in the menstrual cycle, the patient is advised to use barrier methods such as a male external condom, for the duration of a week. After the week has passed, the medication will be fully effective in the person’s body and they will not need another form of birth control.4, 5

The birth control implant is surgically implanted by a medical professional just under the skin on the inside of the upper arm. During the procedure, the individual receiving the implant will lie on their back with their non-dominant arm flexed at the elbow. The insertion site is disinfected and the medical professional gives the arm a shot to numb the area where the implant will be inserted. The implant is then inserted with a tool to slide it under the skin. Most people only feel a pinch when receiving the shot, and do not feel the implant being inserted. The implant is inserted just under the skin in the inner part of the upper non-dominant arm, an area distant from blood vessels and nerve structures so that it is unlikely to cause damage to the arm.6 It is extremely important to have the implant inserted by a trained medical professional in order to avoid any problems and to ensure that the device works properly. Following insertion of the implant, individuals can have sex, but must consult with their doctor to verify the date that the implant will begin working in the body.4
For up to two weeks after insertion, it is possible to have bruising or soreness around the birth control implant.2 This is completely normal and is not a cause for concern. If pain persists for a longer period or is very severe, you should contact your medical care provider.
How Does It Work?
The birth control implant functions primarily through the release of the hormone progestin. Progestin thickens cervical mucus, which creates a barrier for sperm cells that are traveling into the uterus. Blocking the path of sperm consequently prevents fertilization, thus preventing pregnancy. Additionally, progestin can also function by preventing ovulation from occurring. Ovulation is the process by which a mature egg is released and travels out of the ovaries to be fertilized by a sperm cell. By preventing ovulation from taking place, the eggs will not be released and consequently not have the opportunity to be fertilized. Depending on the time of insertion in relation to the individual’s menstrual cycle, the implant can be effective immediately or within a week. After this waiting period is over, the implant is a highly effective method of birth control on its own. However, it is recommended to take other precautions against STI transmission as the implant does not provide this.4, 5
How Effective Is It?
The birth control implant has been shown to be over 99% effective in preventing pregnancy with less than 1 out of 100 people becoming pregnant while using the implant.3 When used for longer than the currently recommended time frame of three years, the implant has been found to continue to be effective for up to five years.1 One study found that there were no pregnancies out of 200 women using the Nexplanon implant for five years rather than the typically recommended three years.6
Part of what makes the birth control implant such an effective method of birth control is that there is less room for user error, as users do not have to remember to take a pill. As long as the implant is inserted correctly and does not move, it will continue to release hormones at a steady, constant rate for at least three years and potentially up to five years.6, 7
How Is the Birth Control Implant Removed?
The birth control implant can be removed at any time after insertion if one no longer wants to use this method of birth control. It is typically recommended by health professionals that the implant is removed after three years, however the implant can be effective for up to five. It is up to the individual and the guidance of their health professional to decide when to remove the implant, whether that be three years, five years, or any time in between.5
The removal procedure must be performed by a healthcare professional and is relatively pain-free. This procedure only takes a few minutes longer than the insertion. During removal, the health care provider will first feel the arm to locate the implant. Although movement of the implant is rare and usually only consists of several millimeters, it is possible that the healthcare provider may not be able to feel the implant. In this case, an ultrasound or X-ray will be performed to locate the implant prior to removal.6 Once the implant is located, the health care provider numbs the area by administering a shot and makes a small incision to remove the implant with sterile surgical forceps.6 During the procedure, individuals have the option of inserting a new implant to continue protection against pregnancy for another three to five years.3 If a person decides not to reinsert a new implant, then pregnancy can occur any time after the implant is removed, including immediately after.3 Following removal, the patient will receive proper care instructions from a medical professional. It is common that the arm may feel sore or bruised temporarily. Because the insertion and removal of the implant is an invasive procedure, it is important to follow proper precautions to ensure the insertion/removal region stays sanitized to prevent any infections.5
It is advised to remove the birth control implant either when it is time to be replaced (the end of the 5-year mark) or when the user is ready to have children or switch to another birth control method. Once removed, the hormones in the implant will no longer be released in the body, allowing ovulation to continue. Consequently, the patient can become pregnant as soon as the implant has been removed, making it an effective and reversible method. Concurrently, if the implant is not replaced, any side effects associated with the drug will stop soon after the removal.5

A common concern with many birth control methods is their impact on the patient’s fertility. There is little to no data supporting the idea that Nexplanon negatively impacts one’s fertility. It is a safe and healthy method of birth control. In fact, a 2020 study collected data from about 18,000 people with vulvas and found that those who had intrauterine devices and implants had the quickest return of fertility in comparison to other popular forms of birth control (the pill, vaginal ring, and Depo-provera shot). On average, these individuals had to wait for about two menstrual cycles until they could become pregnant. To compare, individuals in the study who reported using other methods such as a daily pill or vaginal rings did not become pregnant until about three menstrual cycles had passed. Individuals using other forms of birth control such as the Depo-Provera shot and the patch had to wait even longer. This study concluded that these forms of contraception, the implant included, did not have any lasting effect on the patient’s fertility. So, while it may take time for pregnancy to occur following the removal of the implant, fertility is very likely to return to normal.8
How Much Does It Cost?
Depending on a person’s insurance, insertion of the birth control implant can cost anywhere from $0 to about $1,030 and removal can cost between $0 and $300.2, 5 Although it can be a high upfront cost, the implant is very cost-effective since it prevents pregnancy for up to five years.1 Health centers such as Planned Parenthood can connect individuals interested in the implant with resources to access birth control at a low or no cost; if you live in the United States, you can find your local Planned Parenthood by clicking here. Some individuals in the United States may also be able to get Nexplanon for free through the birth control coverage offered by the Affordable Care Act.3
What are the Benefits of the Birth Control Implant?

The implant has several advantages over other forms of contraception:
- It can be removed at any time and is reversible, meaning that users can get pregnant soon after its removal. Etonogestrel, the synthetic hormone used in the implant, was shown to be undetectable in the blood one week after removal.9
- It can be used while breastfeeding without altering an individual’s ability to lactate. 10
- It can be inserted directly following birth, abortion, or miscarriage to avoid unintended pregnancy.11
- It is convenient and does not require daily or weekly action by the user to ensure effectiveness.3
- It is one of the most effective forms of birth control.3
- It provides long-lasting birth control that does not involve sterilization.3
- It does not contain estrogen.3
- It can be cost-effective, depending on an individual’s insurance situation. In the United States, the Affordable Care Act may provide a way for some individuals to get Nexplanon for free.3
The implant can be very appealing to people who cannot take estrogen and who want a long-lasting and low maintenance form of contraception. The implant’s reversibility is also very appealing to people who would like to become pregnant soon after the removal of the implant.
What are the disadvantages?

While the implant is a great and viable option for many individuals, it may not be for everyone. As like any drug, it has its potential disadvantages. One downside to the implant is the invasive insertion process. While it does not require extensive surgery, it does often require a local anesthetic to numb the area along with a minor puncture of the skin. The process does not take long and is not reported to be excruciatingly painful, but it can pose slight pain and discomfort which may deter many potential users as there are other birth control options that do not require a medical professional. Furthermore, it is required that users of the implant make an appointment to see a medical professional in-person for both the insertion and removal.4
Another crucial disadvantage to the implant is its lack of STI protection. The only birth control method that can also protect against STIs is the condom. However, this barrier method can be paired with the implant for dual protection against pregnancy and now protection against any STIs. Because of its high efficacy in preventing pregnancies, many people may not feel the same sense of urgency to simultaneously use a condom–thus it is safest to test frequently for STIs and/or use a condom for ultimate protection.4
There is also the possibility of a failed insertion or removal. In rare cases, the medical professional may not be able to complete the insertion properly or find the implant during removal, which may require a more complicated surgery in the hospital. Other complications including pain, infection, and scarring may occur. Another unlikely scenario is the possibility of the implant coming out by itself, which would require another visit to a doctor to have it reinserted, as once the implant is no longer in the body the user is not protected from pregnancy.5
Another possible disadvantage of the implant is that it is not hormone-free. While it does not use estrogen, some patients might prefer a birth control method that is completely hormone-free such as the copper IUD. Further, like many other medications, the implant comes with a series of potential side effects. Many of these side effects may go away after a few weeks as the body adjusts to the implant. However, everyone’s body is different, and some people may be affected more than others.5
What Are The Risks and Side Effects?
Some side effects of the etonogestrel birth control implant includes irregular periods, the absence of monthly periods (amenorrhea), or periods that are either heavier or lighter than usual.12 Users may also experience spotting between periods.12 Studies have shown that one out of ten women stopped using the implant due to the irregular bleeding that was caused from it.5 There are also possible side effects not related to the menstrual cycle, such as weight gain, headaches, acne, changes in breast tenderness, and depression.13
If an implant user is experiencing potentially dangerous side effects, they should contact a medical professional immediately. These side effects include changes in vaginal discharge, a moving implant, ejection of the implant, redness, pus, or pain at the insertion site, severe headaches, prolonged menstrual bleeding, and yellowing of the skin or eyes. 7,13
Although rare, it is possible that pregnancy can occur while using Nexplanon, as it does not provide 100% protection.2, 4 In the case that this occurs, individuals who experience pregnancy have a higher chance of having an ectopic pregnancy, a pregnancy that occurs outside the uterus. Ectopic pregnancies require more visits to the doctor as they can cause many health complications such as internal bleeding, infertility, and more.2, 5
Similarly to other birth control methods, using Nexplanon may increase an individual’s odds of developing blood clots. For this reason, it is highly advised that users avoid smoking tobacco products as these can further increase the odds of developing a blood clot. Implant users may also experience cysts, headaches, vaginal inflammation, acne, and more.5
When to Avoid the Birth Control Implant
Usage of the implant can lead to health complications in some specific circumstances. Individuals experiencing these circumstances should not use the birth control implant:

- Are pregnant or think they may be pregnant.3
- Have a history of blood clots.3
- Have liver disease or liver tumors.3
- Have unexplained vaginal bleeding.3
- Currently have or have had certain types of cancer such as breast cancer and other progestin-sensitive cancers. 3
- Are allergic to any substance in the implant.3
Individuals considering using the Nexplanon implant should always speak to a doctor about their health history and any health conditions they may have. If they are unsure about whether they have a health condition or not, it is advised to speak to a doctor, as well as ask if the birth control implant is appropriate for their situation.
Concluding Remarks
The birth control implant offers many benefits and is extremely effective at preventing pregnancy. However, it does not provide any protection against sexually transmitted infections (STIs), so it is recommended that the implant be used in conjunction with barrier methods such as external or internal condoms. Insertion of the implant is a simple procedure that takes only a few minutes and provides at least three years and up to five years of contraception.1 The implant is one of the most effective forms of contraception and offers easy and convenient use.
References
- Mcnicholas, Colleen, Erin Swor, Leping Wan, and Jeffrey F Peipert. “Prolonged Use of the Etonogestrel Implant and Levonorgestrel Intrauterine Device: 2 Years beyond Food and Drug Administration–approved Duration.” American Journal of Obstetrics and Gynecology. Vol. 216, no. 6. June 2017.
- “Birth Control Implant.” Planned Parenthood. (n.d).
- “NEXPLANON (Etonogestrel Implant) 68 Mg Radiopaque.” Nexplanon. (n.d.).
- “Contraception Implant.” NHS. 9 March 2021.
- “Nexplanon (etonogestrel implant).” FDA: Access Data. P. 3-7.
- Palomba, Stefano, Angela Falbo, Annalisa Di Cello, Caterina Materazzo, and Fulvio Zullo. “Nexplanon: The New Implant for Long-term Contraception. A Comprehensive Descriptive Review.” Gynecological Endocrinology. Vol. 28, no. 9. 01 Sep. 2012.
- Hirsch, Larissa. (2018, June). “Implantable Contraception.” TeensHealth from Nemours. June 2018.
- Yland, Jennifer J et al. “Pregravid contraceptive use and fecundability: prospective cohort study”. BMJ. Vol. 371. 11 Nov. 2020.
- Ali, Moazzam, Ayse Akin, Luis Bahamondes, Vivian Brache, Ndema Habib, Sihem Landoulsi, and David Hubacher. “Extended Use up to 5 Years of the Etonogestrel-releasing Subdermal Contraceptive Implant: Comparison to Levonorgestrel-releasing Subdermal Implant.” Human Reproduction. Vol. 31, no. 11. Oxford University Press: Nov. 2016.
- Turok, David K, Lawrence Leeman, Jessica N Sanders, Lauren Thaxton, Jennifer L Eggebroten, Nicole Yonke, Holly Bullock, Rameet Singh, Lori M Gawron, and Eve Espey. “Immediate Postpartum Levonorgestrel Intrauterine Device Insertion and Breast-feeding Outcomes: A Noninferiority Randomized Controlled Trial.” American Journal of Obstetrics and Gynecology. Vol. 217, no. 6. Dec. 2017.
- Curtis, Kathryn M, Tara C Jatlaoui, Naomi K Tepper, Lauren B Zapata, Leah G Horton, Denise J Jamieson, and Maura K Whiteman. “U.S. Selected Practice Recommendations for Contraceptive Use, 2016.” MMWR. Recommendations and Reports: Morbidity and Mortality Weekly Report. Recommendations and Reports. Vol. 65, no. 4. July 2016.
- Mansour, Diana, Tjeerd Korver, Maya Marintcheva-Petrova, and Ian S Fraser. “The Effects of Implanon® on Menstrual Bleeding Patterns.” The European Journal of Contraception & Reproductive Health Care. Vol. 13, no. S1. 2008.
- Blumenthal, Paul, Kristina Gemzell-Danielsson, and Maya Marintcheva-Petrova. “Tolerability and Clinical Safety of Implanon®.” European Journal of Contraception & Reproductive Health Care. Vol. 13. 2008.
Last Updated: 24 May 2022.
