Table of Contents
Overview
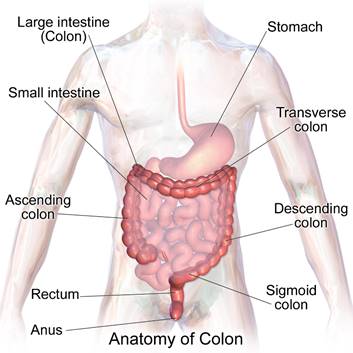
Colon cancer, also called colorectal cancer, is a cancer that occurs in either the colon or the rectum. Both the colon and the rectum are located in the lower abdominal cavity beneath the stomach. The colon is often referred to as the large intestine and the rectum is the passageway that connects the large intestine to the anus (see picture).1 Of the cancers that affect both men and women, colon cancer is the second leading cause of cancer deaths in the United States, killing over 51,000 people each year.1 The good news is, the number of deaths from colon cancer has been steadily decreasing for several decades as people become more aware of the risk factors and the simple screening processes that can detect colon cancer before it becomes deadly.2
Causes and Risk Factors
Almost all colorectal cancers are caused by polyps (abnormal growths) inside the lining of the colon or rectum. These polyps can be present in the colon for years before they actually become cancerous.1
There are many factors that can increase your risk of getting colon cancer, including:
Age – Your risk of getting colon cancer increases as you become older. Colon cancer can occur in younger people, but over 90% of cases occur in people who are 50 years old or older.1
Personal or family history – Your risk of getting colon cancer increases if you have been diagnosed with colon cancer before, or if anyone in your family has been diagnosed with colon cancer at some point in their lives.1
Other Diseases – Your risk of getting colon cancer increases if you have another condition such as Inflammatory Bowel Disease (including Crohn’s disease and ulcerative colitis). People with diabetes and insulin resistance have an increased risk of colon cancer.3
Lifestyle Choices – Your risk of getting colon cancer increases if you have a diet high in fat and low in fruits, vegetables, and fiber. Your risk also increases if you do not exercise regularly, if you are obese or overweight, or if you regularly consume alcohol or tobacco.3
If you have any of these risk factors, it is important that you talk to a doctor.
Symptoms
Common symptoms of colon cancer include:
- Blood in your stool
- Abnormal bowel movements, including diarrhea or constipation
- Persistent stomach pain, aches, or cramps that don’t go away
- Unexplained weight loss
However, these symptoms may be caused by a number of conditions other than colon cancer, so it is important to talk to your doctor about any symptoms that you are experiencing. While these are the most common symptoms, is important to remember that colon cancer may not cause any symptoms and therefore you may not know you have colon cancer, unless you go to the doctor and get screened regularly.3
Screening and Diagnosis
Colon cancer can be detected early with routine screenings. Screenings can detect the precancerous abnormal growths in the colon or rectum, called polyps. Finding a polyp early during screening, before it has the chance to grow and advance to the later stages, is important.1 There are various screening tests that look for colon cancer:
Fecal Occult Blood Testing (FOBT) – This test requires you to provide a stool sample which is then tested with various chemicals to check for the presence of blood. It is recommended that you get a FOBT once a year, after the age of 50.
Sigmoidoscopy – In this test, the doctor inserts a short, thin, flexible tube with a video camera at the end through your anus and into your rectum to check for polyps inside the rectum and lower portion of the colon. It is recommended that you get a sigmoidoscopy once every 5 years, after the age of 50.
Colonoscopy – This test is similar to a sigmoidoscopy, but it uses a longer, thin, flexible tube with a video camera at the end that can check the rectum and the entire length of the colon for polyps. It is recommended that you get a colonoscopy once every 10 years, after the age of 50.
Double-Contrast Barium Enema – In this test, you receive an enema with a liquid substance called barium and then the doctor takes an X-ray of your colon. This chemical makes it easier for doctors to see your colon on the X-ray.
While the four methods discussed above are the most common screening procedures, there is a wide variety of tests available and you should consult with a doctor to determine which screening test is best for you.1
If you test positively for colon cancer on any of these measures, your doctor will run additional tests to determine the stage of colon cancer you have.
The stages include:
Stage 1 – Your cancer has grown through the mucosa lining of the colon or rectum but has not spread outside the colon wall or rectum
Stage 2 – Your cancer has grown through the wall of the colon or rectum but has not spread to nearby lymph nodes
Stage 3- Your cancer has spread to nearby lymph nodes but has not spread to other parts of the body
Stage 4 – Your cancer has spread to other organs
As with many cancers, diagnosis at an earlier stage is important as it leads to a much better prognosis.3
Treatment
Treatment options for colon cancer depend on the stage of the cancer and the overall health of the patient. For early stage cancers, surgery is often the best option. If the polyp is small enough, the doctor may be able to remove it during a colonoscopy.
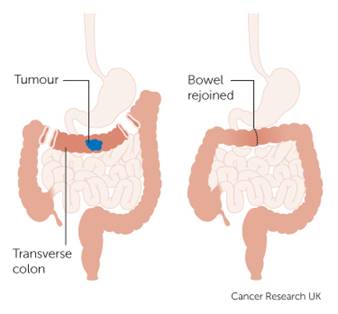
For cancers in stage 2 or 3, a colectomy is recommended. In this surgical procedure, a doctor essentially removes the infected portion of your colon (as well as some surrounding tissue, just to be sure all the cancerous cells have been removed) and reconnects the healthy sections (see picture Left).3
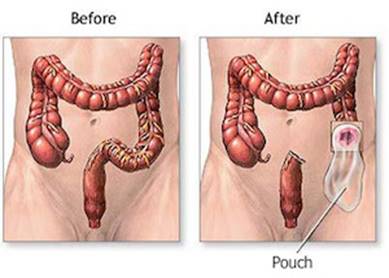
For patients whose cancer is near the rectum and a colectomy is not an option, a colostomy can be a lifesaving surgery. A colostomy involves creating a surgical opening in the lower portion of the colon or rectum and inserting a tube for the feces to be eliminated. This tube starts in the colon and exits the body through the abdomen, and the waste is collected in a special bag outside the body (see picture Right).3 The colon and rectum beyond the site of the colostomy are disconnected or removed and the anus is no longer the exit for stool. Colostomies can be temporary or permanent, depending on your specific case.
Chemotherapy and radiation are also options for patients whose cancer has spread to their lymph nodes and other body parts. If found early, colon cancer can be treated and cured with rather high success rates.
Prevention
In terms of lifestyle factors, many doctors recommend exercising regularly, avoiding heavy alcohol and tobacco use, and maintaining a diet low in animal fats and high in fruits, vegetables, and whole grains. The best way to prevent colon cancer, however, is to have regular screening tests, beginning at age 50. Abnormal growths found during these screenings can be removed before they even become cancerous.1
How Colon Cancer can Affect your Sex Life
For the most part, colon cancer does not have any long term effects on a person’s ability or desire to have sex. Many people may choose not to engage in sex during treatment, particularly as they are going through chemotherapy or immediately after surgery, because they often feel very fatigued. Once a person fully recovers from their surgery or other treatment (usually around 6 weeks), their sex life usually returns to normal. However, there is a small chance that surgery for colon cancer can cause damage to the nerves connected to the sex organs. Because of this, some people may experience some sexual difficulties during intercourse including the inability to get or keep an erection, vaginal dryness, pain during intercourse, or vaginal tightening. However, the biggest effect that colon cancer has on a person’s sex life is in their ability to have anal sex. Some surgeries for colon cancer, including a colostomy, involve permanently removing the lower portion of the rectum and the anus, making it impossible to have anal sex. Other people may feel self-conscious after treatment and not want to engage in anal sex. If anal sex is an important part of your sex life, communicating with your partner about alternative options is very important. Additionally, you and your partner may find it helpful to talk to a sex therapist about your situation.4
Concluding Remarks
While some people may be embarrassed to talk about things related to their colon and rectum, it is important to communicate with your doctor if you are experiencing any abnormal symptoms as they could be indicative of colon cancer. Having regular screening tests is very important because, as with most cancers, catching the disease early is crucial. Being aware of the risk factors and the simple screening processes can significantly decrease your chances of developing colon cancer and help you lead a long, healthy life.
References
- “Colorectal (Colon) Cancer.” Centers for Disease Control and Prevention. 04 Jan. 2016. Web. 31 Jan. 2016. http://www.cdc.gov/cancer/colorectal/index.htm.
- “Colorectal Cancer.” American Cancer Society. N.p., Oct. 2015. Web. 31 Jan.2016. http://www.cancer.org/cancer/colonandrectumcancer/.
- “Colon Cancer.” Mayo Clinic. N.p., 22 Aug. 2013. Web. 31 Jan. 2016. http://www.mayoclinic.org/diseases-conditions/colon-cancer/basics/definition/con-20031877
- “Sex and Bowel Cancer.” Cancer Research UK. N.p., n.d. Web. 20 Feb. 2016. http://www.cancerresearchuk.org/about-cancer/type/bowel-cancer/living/sex-and-bowel-cancer
Last Updated 08 March 2016.
