Ovarian cancer is a type of cancer that affects the female reproductive system. It generally begins in one of the two ovaries on either sides of the uterus and can often remain undetected for most of the beginning stages. Ovarian cancer is usually identified once it has metastasized (spread) to other parts of the pelvic area and abdomen.3 Ovarian cancer is relatively uncommon, with only around 1.3% of women receiving a diagnosis in their lifetime.4
Types Of Ovarian Cancer
There are a number of different types of ovarian cancers, some of which vary in frequency in at-risk populations, diagnosis methods, and difficulty to treat.3
Epithelial Ovarian Cancer (EOC)
Most ovarian cancers fall into this category. Epithelial ovarian cancer (EOC) usually starts in the surface layer covering the ovary. Cancerous tumors in epithelial ovarian cancer are often composed of four cell types, or adenomas: serious, mucinous, clear cell, and endometrioid. When the deoxyribonucleic acid (DNA) within these cells mutates, it can lead to uncontrolled cell division (i.e., cancer).
- Serous adenomas: The most common type of epithelial ovarian cancer is the serous cell type, and research has found that serous cells usually become cancerous in the fallopian tube first, after which they migrate to the surface of the ovary.
- Mucinous adenomas: These types of adenomas occur in 7-14% of all patients with epithelial ovarian cancer. Studies have found that while this type of ovarian cancer is relatively rarer, it also tends to have worse rates of response to chemotherapy (i.e., chemoresistance) in the advanced stages than other types of ovarian cancer. Fortunately, mucinous adenomas are frequently detected and diagnosed earlier than other forms of adenomas.1
- Clear-cell adenomas: These types of cells make up less than 5% of all epithelial ovarian cancers. Another name for these are ovarian clear-cell carcinomas, or OCCCs, and they have been described by the World Health Organization (WHO) as transparent cells growing in clusters in various parts of the pelvic area.1 OCCCs often appear as large masses and can sometimes be felt during gynecologic exams. Currently, advanced stage OCCC has a relatively low survival rate, because similar to mucinous ademonas, this type of ovarian cancer exhibits some chemoresistance.
- Endometrioid adenomas: These types of cells make up about 20% of all EOCs (epithelial ovarian cancers). Generally, females who develop this form of carcinoma tend to be younger and will also have a better 5 year and 10 year survival rate.2
Ovarian Low Malignant Potential Tumor (OLMPT)
These are also known as borderline tumors, and they make up about 15% of ovarian cancers. The tumors generally consist of serous or mucinous cell types, and unlike most malignant tumors, they rarely spread. Because of this, OLMP tumors can be removed with surgery, and no further radiation or chemotherapy is necessary for treatment.
Germ Cell Ovarian Cancers
This type of tumor is fairly uncommon and is observed primarily in teenagers and young women. There are a number of different subcategories within this group, since these tumors arise from undifferentiated ovarian reproductive cells.
Stromal Ovarian Cancers
These cancers arise from the ovary itself and are very uncommon. Some examples include granulosa-stromal tumors and Sertoli-Leydig tumors.
While there are numerous categories that have yet to be discovered, researchers have been able to broadly categorize ovarian cancers within the listed above groups.
Risk Factors
There are a number of risk factors that increase an individual’s chance of developing ovarian cancer. These factors have been grouped into three large categories: menstrual cycles, family history, and lifestyle choices.4
Menstrual Cycles and Ovulation
Females who ovulate more frequently are at a higher risk for developing ovarian cancer. Additionally, females who start their period earlier, ended their period and entered menopause later in life, and/or experience symptoms of infertility are at a greater risk of ovarian cancer.
Genetic Predisposition and Family History
According to current research, about 15% of ovarian cancers are genetically related. The BRCA1 and BRCA2 gene are very important as tumor-suppressor genes, and when they undergo mutations, it can greatly increase the risk of cancer. Females withthe BRCA1 gene mutation have a 39% chance of developing ovarian cancer in their lifetime. Individuals can get tested for this mutation via a simple blood test, which can greatly affect the way family members choose to monitor their health. Additionally, the risk of ovarian cancer becomes higher as an individual gets older. In fact, half of all ovarian cancers are found in women 63 years of age or older.3 If there is a family history of specifically ovarian, breast, or colorectal cancer, this can also increase the risk of ovarian cancer. This is because different cancers can be linked to the same gene mutation, especially if that gene is one involved in tumor suppression.3
Lifestyle
The use of birth control, such as oral contraceptives and the Depo-Provera shot, have been known to actually reduce the risk of ovarian cancer. The lower risk was maintained years after stopping birth control.3 Some fertility drugs, e.g., clomiphene citrate, may increase the risk of ovarian tumors, along with drugs that increase androgen and estrogen levels in the body. Androgen and estrogen are male and female hormones, respectively.3 Regarding lifestyle choices, recent studies have shown that females who followed a low fat diet for at least four years were at lower risk of ovarian cancer. 3
The etiology of ovarian cancer has not been narrowed down to an exact cause; however, combinations of certain risk factors, along with varying degrees of severity of those factors can determine whether an individual develops ovarian cancer in their lifetime.
Symptoms
Ovarian cancer can have vastly varying signs and symptoms, which can make the condition difficult to diagnose. Some of these symptoms include 3:
- Bloating
- Pelvic or abdominal pain
- Trouble eating or feeling full quickly
- Urinary symptoms (urgency and frequency)
- Fatigue
- Upset stomach
- Pain during sex
- Constipation
However, it can be difficult to know if these symptoms are caused by more common, milder conditions, or if they indicate to a more serious issue. Because of this, biopsies and other, more specific exams can identify and analyze large masses in the ovary and pelvic region.
Detection
Ovarian cancer can be detected in a number of ways. Many of these depend on the stage to which the cancer has progressed.3
Physical Exam
A physician will do a pelvic exam and look for telltale signs of ovarian cancer. Some examples of these include an enlarged ovary or signs of fluid in the abdomen (known as ascites.)3
Specialist Consultation
If any of the patient’s test results are abnormal, a physician may refer them to a medical professional who specializes in treating ovarian cancer specifically. Doctors that treat cancers of the female reproductive tract are called gynecologic oncologists. Once this physician runs a number of specialized tests, they often take on the responsibility of care, which includes creating a diagnostic and treatment plan.3
MRIs, CT Scans, and Ultrasounds
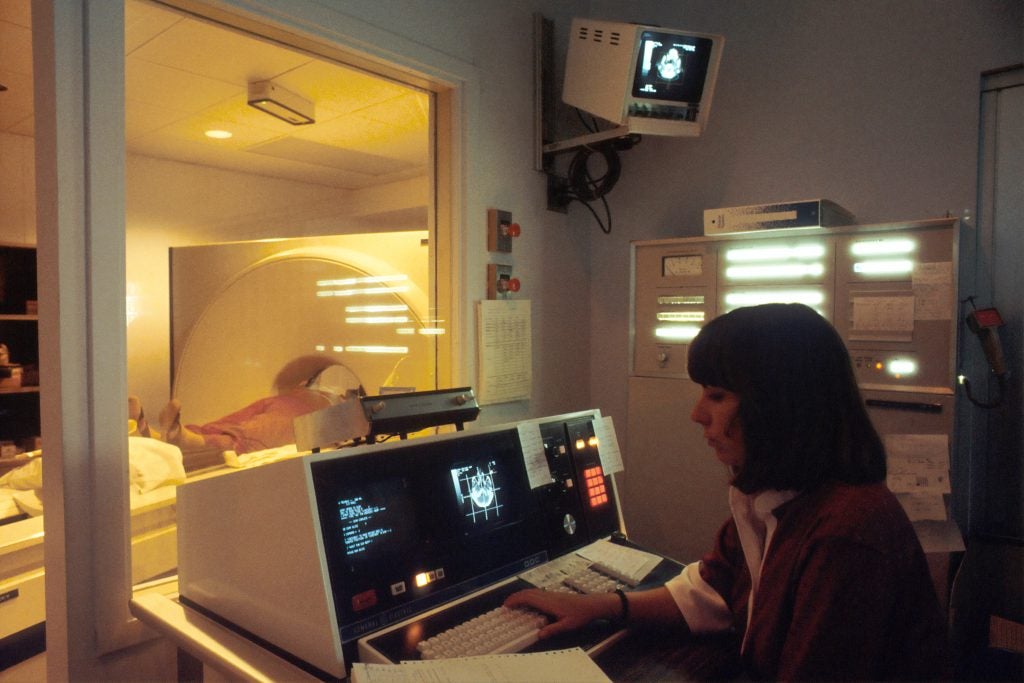
These three imaging techniques are very important in the diagnostic process, as they can help confirm the presence of a mass and see if and where it has spread.
MRIs: Magnetic Resonance Imaging (MRI) scans are a complex form of imaging where body tissues absorb radio waves and emit them in various patterns that are characteristic to certain diseases. These are used very rarely when looking for ovarian cancer.
CT scans: These scans are very similar to x-rays, except that the machine rotates around the patient while continuously taking pictures. These scans take longer than traditional x-rays and are most useful for detecting large tumors and enlarged lymph nodes. Enlarged lymph nodes are a common sign that any present ovarian tumors are spreading to other organs.
Ultrasound: This is generally the first test done if any abnormality in the ovaries is suspected. Sound waves are transmitted from a probe that is either placed in the vagina or on the abdomen, and these waves create echoes that form a picture on the ultrasound technician’s computer. This type of imagine is very useful to find ovarian tumors as well as confirming what type of mass it is (e.g., a solid tumor or a fluid-filled cyst.) This information is crucial to an oncologist who is trying to create the most successful course of action.3
Laparascopy
This procedure involves inserting a camera that is attached to the end of a thin tube into the lower abdomen. The camera is placed within a fiber-optic instrument, and is carefully inserted through a small cut in the abdominal wall. This allows the physician to look at the pelvic organs and see where the primary tumors are and if they have spread.3
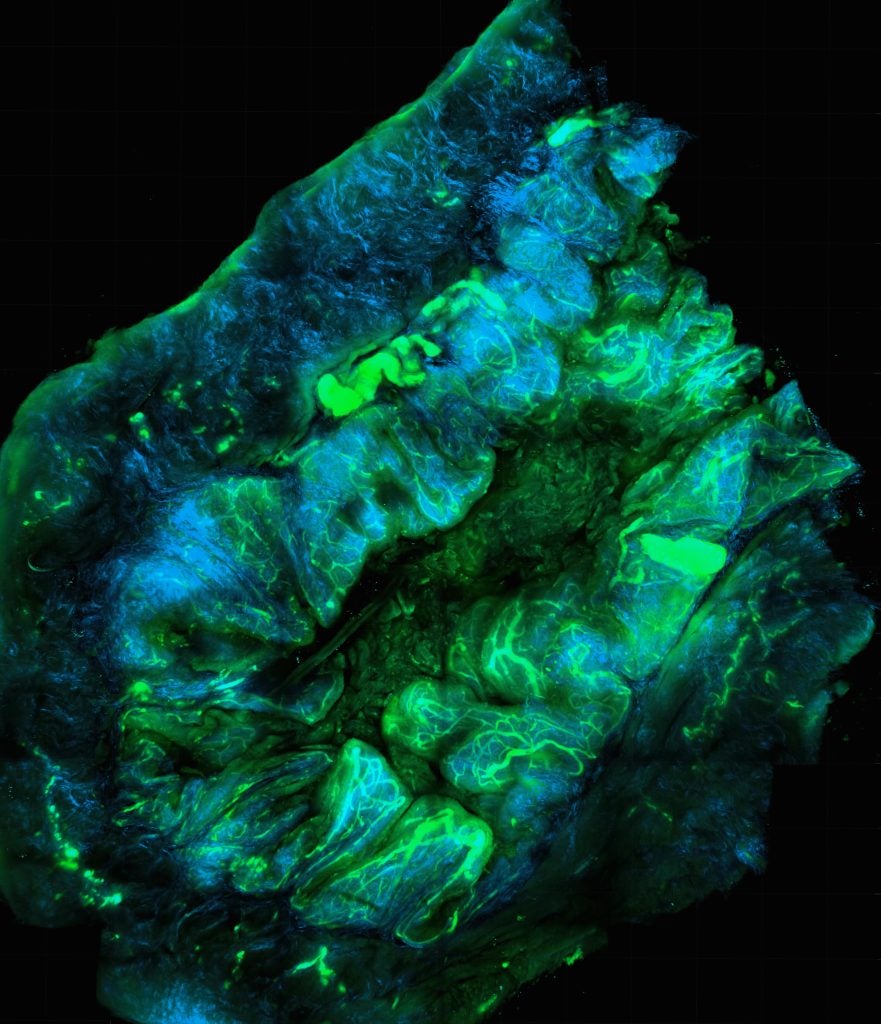
Biopsy
In regards to ovarian tumors, biopsies are usually performed after the tumor has been removed. Biopsies can help identify the composition of a tumor, and whether or not it is cancerous. In very rare cases, biopsies are done while the tumor is still in the body, either because the patient cannot tolerate surgery or because a biopsy would greatly increase the risk of metastasis (i.e., the cancer spreading).3
Blood Tests

A physician may order a full-panel blood test that measures the amount of red blood cells, white blood cells, and clotting factors. These are important indicators of kidney and liver function, which are generally the first systems at risk when ovarian cancer spreads. Additionally, a physician may order a CA-125 test as increased levels of this factor in the blood are associated with a high risk of gynecologic cancer.
Specifically, some germ cell cancers may increase levels of specific tumor markers in the blood, including human chorionic gonadotropin (HCG), alpha-fetoprotein (AFP), and/or lactate dehydrogenase (LDH). Stromal tumors can cause elevated levels of inhibin and the hormones estrogen and testosterone. A blood test can help identify all of these risk factors.3
Treatment
Treatment for ovarian cancer generally involves surgery to remove as much of the tumorous tissue as possible. Other treatment courses include chemotherapy, hormone therapy, or radiation therapy to eliminate remaining cancer cells.
Surgical Treatment
This form of treatment attempts to remove all visible disease in the abdomen. Another term for this treatment is “surgical debulking.” 3 The surgeries can target a number of different areas, including the uterus, fallopian tubes and ovaries, omentum, and certain parts of the bowel. A hysterectomy is when the uterus, tubes, and ovaries are removed, and an omentectomy is the removal of the large fat pad that hangs off the colon. Depending on how many nodes have developed, this can be a very time-consuming procedure. Recent research has shown that if all visible masses cannot be removed during the surgery, then administering chemotherapy for three cycles before the procedure will likely be just as effective as the surgery itself. After this, any remaining necessary surgery will be far more effective.4
Chemotherapy
If a patient is in good enough health, chemotherapy might be one of the more effective options to treat ovarian cancer. The two drugs most commonly used to target ovarian cancer are carboplatin and paclitaxel, which tend to have fewer side effects. These drugs are administered intravenously, or via the intraperitoneal route. The latter is through the abdomen and has demonstrated promising survival rates.4
Hormone therapy
This type of treatment is usually used to treat ovarian stromal tumors.3
- Lutenizing hormone-releasing hormone agonists turn off estrogen production in the ovaries and are injected every 1 to 3 months.4
- Tamoxifen, while often used to treat breast cancer, can treat ovarian stromal tumors. It also combats estrogen production in body tissues and controls cancerous cell growth.
Aromatase inhibitors block specific enzymes that are responsible for turning hormones into estrogen.
Radiation Therapy
Radiation therapy targets cancer cells with high energy particles.4
- External beam radiation therapy emits from a machine that focuses on the cancer cells from outside the body. This is the primary form of radiation used to target ovarian cancer, and each procedure is only a few minutes long, like an actual x-ray.
- Brachytherapy is when radioactive treatment materials are placed internally, close to the cancer. This is a very rare form of treatment for ovarian cancer.3
Support Systems
Survivors of ovarian cancer may encounter emotional side effects, such as anxiety, fear, and depression. It’s important to treat these aspects of the disease as well through support groups and self-care measures. These groups can be found in hospitals and specialized treatment centers. It’s important for cancer patients and survivors to build a strong system of caring, dependable family and friends. This can greatly speed up their emotional and physical recovery, and allow them to works towards a healthy, positive life.5

Concluding Remarks
With ever improving treatments and therapies available, the rates of remission from ovarian cancer become better every year. With the strong core group of clinical specialists, family, and friends, it is more than possible to live a positive and fulfilling life, even with a diagnosis of ovarian cancer.
References
- “Article Tools.” Journal of Clinical Oncology.
- “Endometrioid Ovarian Cancer Presents Earlier, Offers Better Survival Than Serous Carcinoma.” Cancer Network | The Oncology Journal, 20 Jan. 2017,
- “Ovarian Cancer.” American Cancer Society.
- “Ovarian Cancer Causes.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 12 June 2014.
Last Updated: 4 March 2018.
