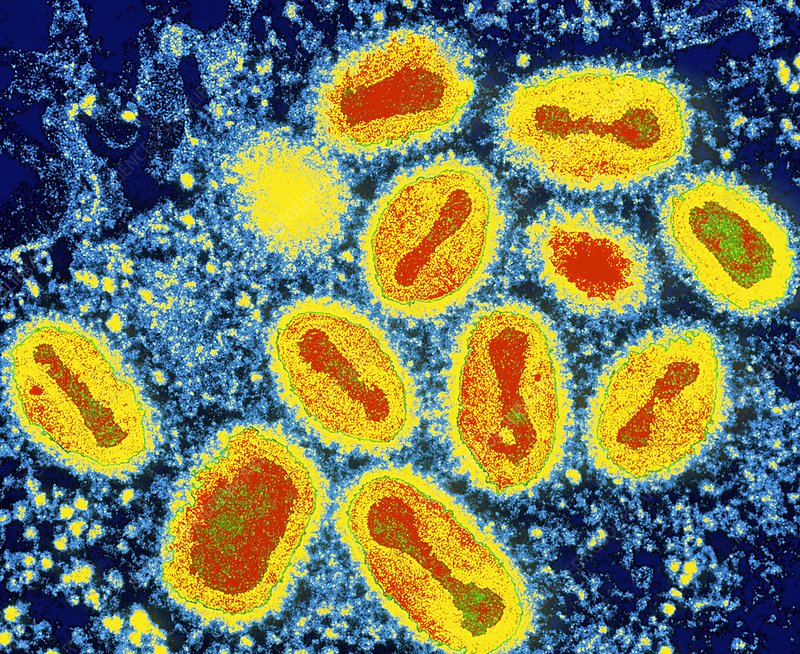
Molluscum contagiosum is a viral skin infection caused by the molluscum contagiosum virus (MCV) from the Poxviridae family, which causes pearl-like bumps on the skin. The virus can be transmitted through direct contact with infected skin, indirect contact via objects or materials that carry the virus (e.g., towels, razors, toys, clothing, bedding, gym equipment), and through sexual contact, classifying this condition as a sexually transmitted infection (STI). The virus is most commonly found in small children, sexually active adults, and immunocompromised individuals, but others are also at risk of contracting molluscum contagiosum. Molluscum contagiosum is often considered a mild skin rash.
Symptoms
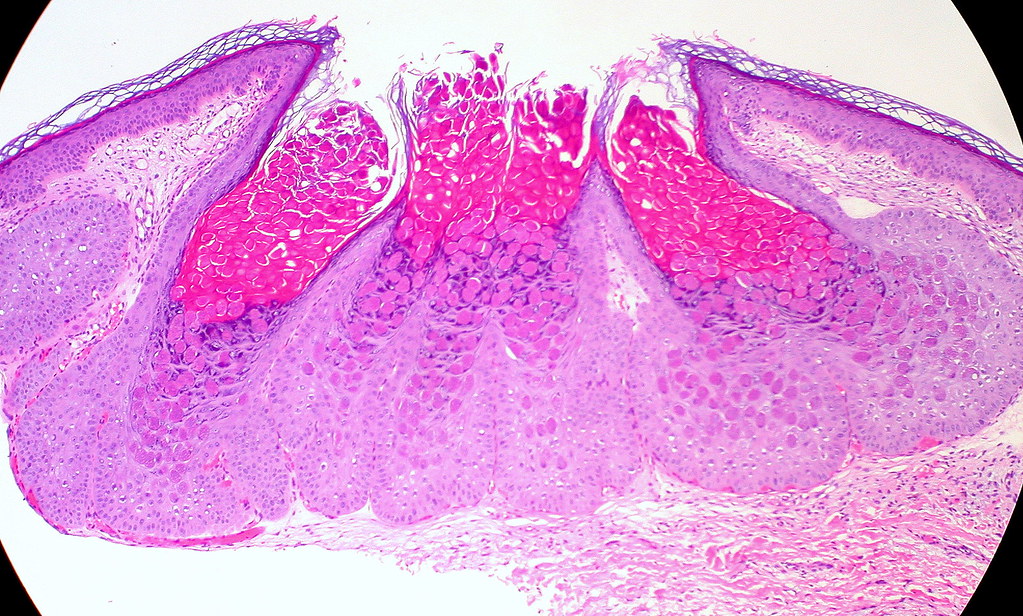
The main symptom of molluscum contagiosum is the appearance of white, pink, or skin-colored bumps that are two to five millimeters (mm) in diameter and painless unless irritated. The lesions, known as Mollusca, may be larger ( >15 mm in diameter) among immunocompromised individuals.3 The bumps are found both singularly and in clusters, and may become itchy, sore, red, or swollen.6 Most patients have between one and 20 lesions, but some have up to hundreds. When found on the genitals, the bumps are typically soft and smooth in texture and contain white, waxy pus.3 Molluscum contagiosum is often confused with herpes, but there are distinct differences between the two conditions. Molluscum contagiosum lesions are painless, whereas herpes lesions have been described as painful. When newly formed, the domes are firm; later, they become soft and gray and may drain fluid. An official medical diagnosis is made by a clinician often after close clinical examination, sometimes requiring tools such as dermoscopy that enable observation of miniscule structures not easily visible. Here at SexInfo, we are not doctors, and thus we are not qualified to give anyone a diagnosis. If you are experiencing symptoms described above, we highly recommend visiting a medical professional to receive a medical diagnosis and possible treatment.
Location
Lesions can be found anywhere on the skin.6 In cases specifically from sexual transmission, they are most frequently found on the lower abdomen, thighs, genitals, and perianal area. From non-sexual transmission, common in children, Mollusca are usually found on the face, neck, underarms, and hands. Lesions do not appear on the palms of the hands and the soles of the feet.6
Transmission
Molluscum contagiosum can spread through indirect contact, direct contact, or through sexual behaviors. Penetrative behaviors like penile-vaginal sex (coitus), oral sex, and anal sex, as well as non-penetrative behaviors such as dry humping or mutual masturbation, are able to spread the infection. A person can spread their own infection, referred to as autoinoculation, from one part of their body to another if they rub or scratch the bumps.7 The virus is commonly spread through sharing or touching an infected person’s towels, bedding, clothing, razors, gym and athletic equipment, toys, stuffed animals, and materials alike.3
Treatment
Individuals who have strong immune systems can expect lesions to take six to 12 months to resolve.3 It can take anywhere from three months to four years for the skin to clear completely.6 However, people who have illnesses resulting in immunodeficiency, such as HIV, may experience much more rapid and severe symptoms because of their bodies’ weakened immune responses. In most cases, clinicians will not prescribe treatments, instead allowing the body to heal itself due to the virus’s generally harmless nature. When infection is particularly severe or other issues and comorbidities are present, healthcare providers may recommend the medical removal of lesions, oral therapies, or topical therapies.

Removal of the Mollusca may be beneficial for some who are infected, especially if the lesions are spreading quickly. While the lesions typically resolve without scarring, many people discover that without treatment, new lesions develop and can spread to other areas of the body or to other people. In such cases, individual lesions may be removed by curettage, surgical scraping, application of trichloroacetic acid or bichloracetic acid, cryotherapy (freezing the lesion with liquid nitrogen), laser removal, or electrosurgery.4 Physical removal of lesions must be done by a professional, requires local anesthetic, and may cause pain, irritation, and scarring. Attempting to remove the lesion on one’s own is not advised, as it risks autoinoculation and spread of the virus to other regions of the body, as well as bacterial infections. Oral treatments exist, namely cimetidine, which is a safe, painless, and well tolerated alternative to physical removal. Cimetidine is a popular treatment option for children with molluscum contagiosum, as it provides an alternative to the discomfort from physical removal. However, the applicability of this treatment is limited as facial Mollusca do not respond to the oral therapy. Alternatively, topical medications, such as those used to remove warts, may be helpful. Acne medications that contain benzoyl peroxide may also help in treating the lesions.2 There are other topical therapies available as well, all which require a prescription and possibly the application by a healthcare provider.4 The virus can only live in the bumps and cannot hibernate in a person’s body once these bumps are gone.
Lastly, treatment options for an individual with immunodeficiency are different. Many of the treatments described above may not work effectively with immunocompromised individuals, and thus, there are treatment alternatives that are specialized to immunocompromised peoples’ needs. Most of these treatments consist of immune system boosting therapies targeted to offset the effects of a low CD4 cell count, which is linked to increased molluscum contagiosum contraction.4 Another treatment option called intralesional interferon is used for more severe molluscum contagiosum cases. However, this treatment includes some undesirable side effects such as flu symptoms, pain at injection site, depression, and lethargy.4 Radiation therapy has also been observed to provide some benefit.4
Prevention

There are many ways people can protect themselves from contracting molluscum contagiosum. Most prevention can be done by infected individuals who are educated on the ways to limit the spread, both to others and through autoinoculation. Individuals who are diagnosed or suspect they may have molluscum contagiosum should wash their hands frequently, cover the lesions with clothing or bandages, and avoid touching lesions or spreading the infection to materials or objects. If contact is made between a lesion and an object that can carry a virus, it should be washed immediately. An infected person should also avoid picking at, scratching, rubbing, or attempting to remove the lesions as this causes new lesions to form and increases the risk of spread.
Measures that non-infectious individuals may take to limit their risk of infection are avoiding direct contact with lesions on an infected partner and communicating openly with partners about STI history and recent testing. Additionally, non-infectious individuals may prefer to avoid sharing materials that are capable of harboring infectious particles, such as towels and washcloths. Further, using condoms properly and consistently is effective in reducing the risk of contracting any sexually transmitted infections. Because molluscum contagiosum is highly contagious, following these precautions can greatly decrease the likelihood of contracting or spreading this virus.5
Concluding Remarks
Molluscum contagiosum is a common and mild skin infection that transmits through indirect or direct contact. This contact may be sexual or nonsexual as well. Molluscum contagiosum is identifiable by small white, pink, or flesh-colored lesions that are found individually or in clusters anywhere on the skin. This viral infection requires a diagnosis by a medical professional and is often left untreated to resolve naturally. However, treatment options exist such as physical removal or oral therapy. There are also many helpful ways to prevent the spread or infection of the virus. If you are infected with molluscum contagiosum, we recommend you visit your healthcare provider if lesions spread, persist, or are causing you pain.
References
- Mayo Clinic. (2020, March 21). Molluscum Contagiosum: Symptoms & causes.
- van der Wouden, J. C., van der Sande, R., Kruithof, E. J., Sollie, A., van Suijlekom-Smit, L. W., & Koning, S. (2017). Interventions for cutaneous molluscum contagiosum. The Cochrane database of systematic reviews, 5(5), CD004767.
- Meza-Romero, R., Navarrete-Dechent, C., & Downey, C. (2019). Molluscum contagiosum: an update and review of new perspectives in etiology, diagnosis, and treatment. Clinical, cosmetic and investigational dermatology, 12, 373–381.
- Centers for Disease Control and Prevention. (2017, October 2). Molluscum Contagiosum: Treatment.
- Hughes, C. M., Damon, I. K., & Reynolds, M. G. (2013). Understanding U.S. healthcare providers’ practices and experiences with molluscum contagiosum. PloS one, 8(10), e76948.
- Centers for Disease Control and Prevention. (2015, May 11). Molluscum Contagiosum.
- Boskey, E. (2020, December 27). When you give yourself a disease. Very Well Health.
Last Updated 27 May 2021.